Table of Contents
ToggleLast updated on August 22, 2025
At Vein Doctors Sydney, we see firsthand how often thrombosis goes undetected until it becomes a serious issue. That’s why recognising the early signs and understanding the different types of thrombosis is so important.
Thrombosis occurs when a blood clot forms inside a vein or artery, disrupting normal blood flow. While some clots dissolve on their own, others can block critical circulation, leading to life-threatening complications like stroke, pulmonary embolism, or limb damage.
Whether you’re managing existing risk factors or simply want to stay informed, this guide will walk you through what thrombosis is, what causes thrombosis, and the main types you should know about. We’ll also cover early warning signs and answer common questions so you’re better prepared to take action if needed.
What Is Thrombosis?
Thrombosis refers to the formation of a blood clot (or thrombus) within a blood vessel – either a vein or an artery. These clots can either stay in place (leading to localised blockage) or break off and travel through the bloodstream, potentially blocking blood flow elsewhere in the body.
When this occurs, normal circulation is disrupted. This can starve tissues of oxygen and nutrients, leading to serious consequences such as stroke, heart attack, pulmonary embolism, or even limb loss, depending on the location and severity of the blockage.
There are two primary types of thrombosis based on where the clot forms:
Venous thrombosis: Clots in the veins, which carry blood back to the heart.
Arterial thrombosis: Clots in the arteries, which carry oxygenated blood from the heart to the rest of the body.
Thrombosis is the result of multiple overlapping factors such as being immobile for long periods of time, vessel wall injury, smoking, obesity and more.
What Causes Thrombosis?
While thrombosis may seem sudden, it’s often the result of multiple overlapping factors. The three major contributors are explained by Virchow’s Triad:
Reduced mobility (stasis) – Blood flows more slowly when you’re immobile for long periods (e.g., after surgery, during long-haul flights, or due to chronic illness), increasing the risk of clot formation.
Hypercoagulable blood – Some people naturally have blood that clots more easily due to genetic conditions, pregnancy, certain medications (like hormone therapy or oral contraceptives), or chronic diseases like cancer.
Vessel wall injury – Damage to a blood vessel from trauma, surgery, or inflammation can also trigger clot formation at the site of injury.
Additional Risk Factors:
- Smoking
- Obesity
- Age (particularly over 60)
- Pregnancy and postpartum period
- Prolonged bed rest or sedentary lifestyle
- Chronic health conditions like diabetes, heart disease, or autoimmune disorders
- Family history of thrombosis or clotting disorders
Understanding what causes thrombosis can help you identify and manage your risk early – especially if you have multiple contributing factors.
Types of Thrombosis You Should Know
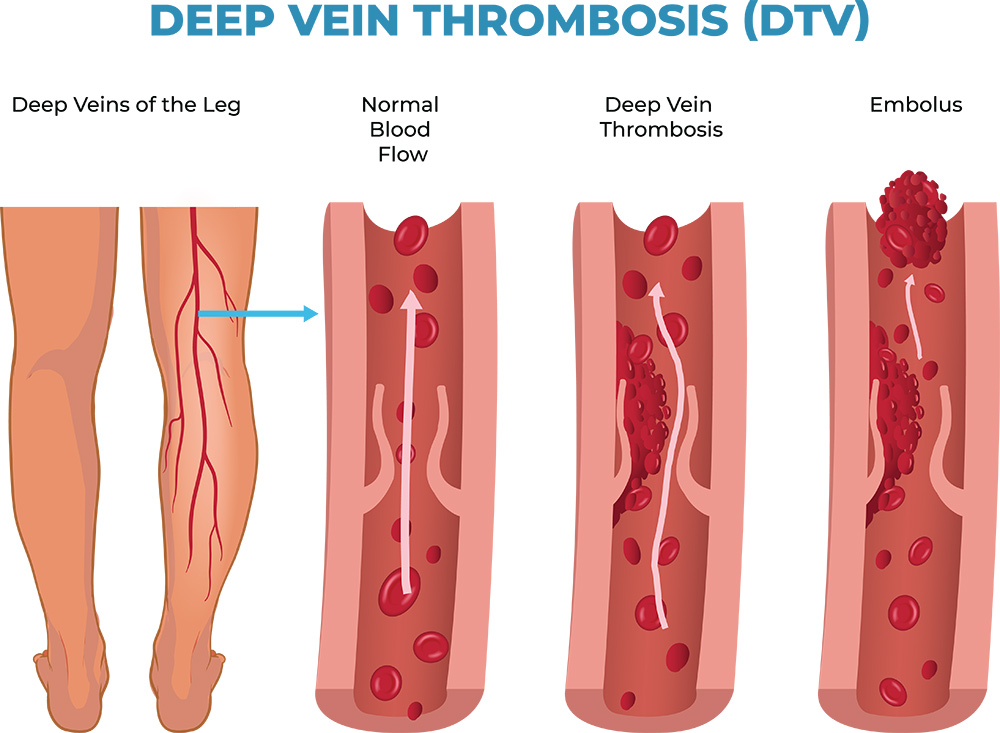
Deep Vein Thrombosis (DVT)
DVT is one of the most common types of venous thrombosis, where a clot forms in the deep veins—most often in the lower leg, thigh, or pelvis. It’s especially dangerous because the clot can break off and travel to the lungs, causing a potentially fatal pulmonary embolism.
Signs and symptoms include:
- Cramping or throbbing pain, typically in one leg (calf or thigh)
- Swelling and warmth in the affected limb
- Red or discoloured skin over the area
- Veins that feel hard or appear more prominent
Pulmonary Embolism (PE)
A pulmonary embolism occurs when a clot—usually originating from a DVT—travels through the bloodstream and blocks an artery in the lungs. It can develop suddenly and is considered a medical emergency.
Warning signs include:
- Sudden shortness of breath
- Sharp chest pain, often worsened by deep breathing
- Rapid heartbeat or palpitations
- Light-headedness, fainting, or coughing up blood
Prompt diagnosis and treatment are critical to avoid long-term lung damage or death.
Superficial Thrombophlebitis
This is a more localised form of thrombosis that affects veins close to the surface of the skin, often in the legs or arms. It’s typically less severe than DVT but may still cause discomfort and inflammation.
Common symptoms:
- A firm, tender, red line along the vein
- Warmth and swelling in the surrounding tissue
- Vein that feels cord-like under the skin
- Mild fever in some cases
Although it’s usually self-limiting, medical evaluation is still advised to rule out deeper involvement.
Arterial Thrombosis
Unlike venous thrombosis, arterial thrombosis involves blood clots in the arteries and can restrict blood supply to critical organs. The outcome can be immediate and severe, such as a heart attack or stroke.
Symptoms vary by location:
Heart: Sudden chest pain or pressure, radiating to the arm or jaw
Brain: Slurred speech, sudden weakness, facial drooping, confusion
Limbs: Coldness, numbness, pale or bluish skin, severe pain
This type of thrombosis often requires urgent medical or surgical intervention.

Thrombosis can be diagnosed through ways such as performing a physical examination, conducting ultrasound imaging or using a CT or MRI scan.
How Is Thrombosis Diagnosed?
To diagnose thrombosis, your healthcare provider may:
- Perform a physical examination for swelling or redness
- Order a D-dimer test to detect clotting activity in the blood
- Conduct ultrasound imaging to check for deeper vein clots (such as in DVT)
- Use computed tomography (CT) or magnetic resonance imaging (MRI) scans for suspected pulmonary embolism (PE) or cerebral venous sinus thrombosis (CVST).
Prompt diagnosis is essential to avoid complications like stroke, PE, or chronic vein issues.
How Is Thrombosis Treated?
The goal of treatment is to restore proper blood flow, prevent the clot from growing, and stop new clots from forming. Options include:
- Anticoagulant medications (blood thinners): These are often the first step in treatment. They help stop existing clots from growing and reduce the risk of new clots forming.
- Thrombolysis: In more urgent cases, a special medication is delivered directly to the clot through a small tube (catheter) to help dissolve it and improve blood flow.
- Endovascular thrombectomy: This is a minimally invasive procedure where a catheter is used to physically remove the clot from the blood vessel. It’s usually done when the clot is large or not responding to medication.
- Compression stockings: These are commonly used to improve circulation, reduce swelling, and lower the risk of complications—especially for clots in the legs.
- Surgical intervention: In rare or severe cases, surgery may be needed to remove the clot or repair the affected blood vessel.
At Vein Doctors Sydney, our team can tailor a treatment plan based on your specific condition and risk level.
How to Book an Appointment
At Vein Doctors Sydney, we are committed to providing personalised and compassionate care for patients seeking relief from thrombosis. For more information on our services or to schedule a consultation at our clinic, please contact our friendly staff by either calling us on (02) 9023 9970, via our online form or by sending us an email.
Frequently Asked Questions
What does thrombosis feel like?
Thrombosis can cause pain or heaviness in the affected area. In the leg (as with DVT), it may feel like cramping, tightness, or a dull ache. You may also feel warmth, tenderness, or notice swollen veins. In the case of arterial thrombosis, symptoms may feel more sudden and intense.
What does thrombosis look like?
In superficial cases, thrombosis may look like a red, raised area or a firm line under the skin. With DVT, visible signs can include swelling, skin discolouration, and enlarged surface veins. However, deeper veins affected by thrombosis may show no outward signs, making early medical evaluation crucial.
Can you have thrombosis without symptoms?
Yes. Some cases, especially DVT, can be “silent” and present no symptoms. That’s why it’s important to be aware of your risk factors and act early if something feels off.
Who is most at risk of developing thrombosis?
Anyone can develop thrombosis, but risk is higher in people over 60, those with a family history of blood clots, individuals who are immobile for long periods, and patients recovering from surgery or trauma.
How can I reduce my risk of thrombosis?
Stay physically active, hydrate well, and avoid smoking. On long trips, move your legs frequently. For higher-risk individuals, your doctor may recommend preventative medications or compression therapy.
This information is not intended to be used for diagnosis or treatment. It is aimed at presenting a perspective only and is not a substitute for a prescription. Anyone experiencing a medical condition should consult their doctor.

